Hirschprung`s disease, a practical approach.
Main Article Content
Abstract
Initially, Hirschsprung's disease was
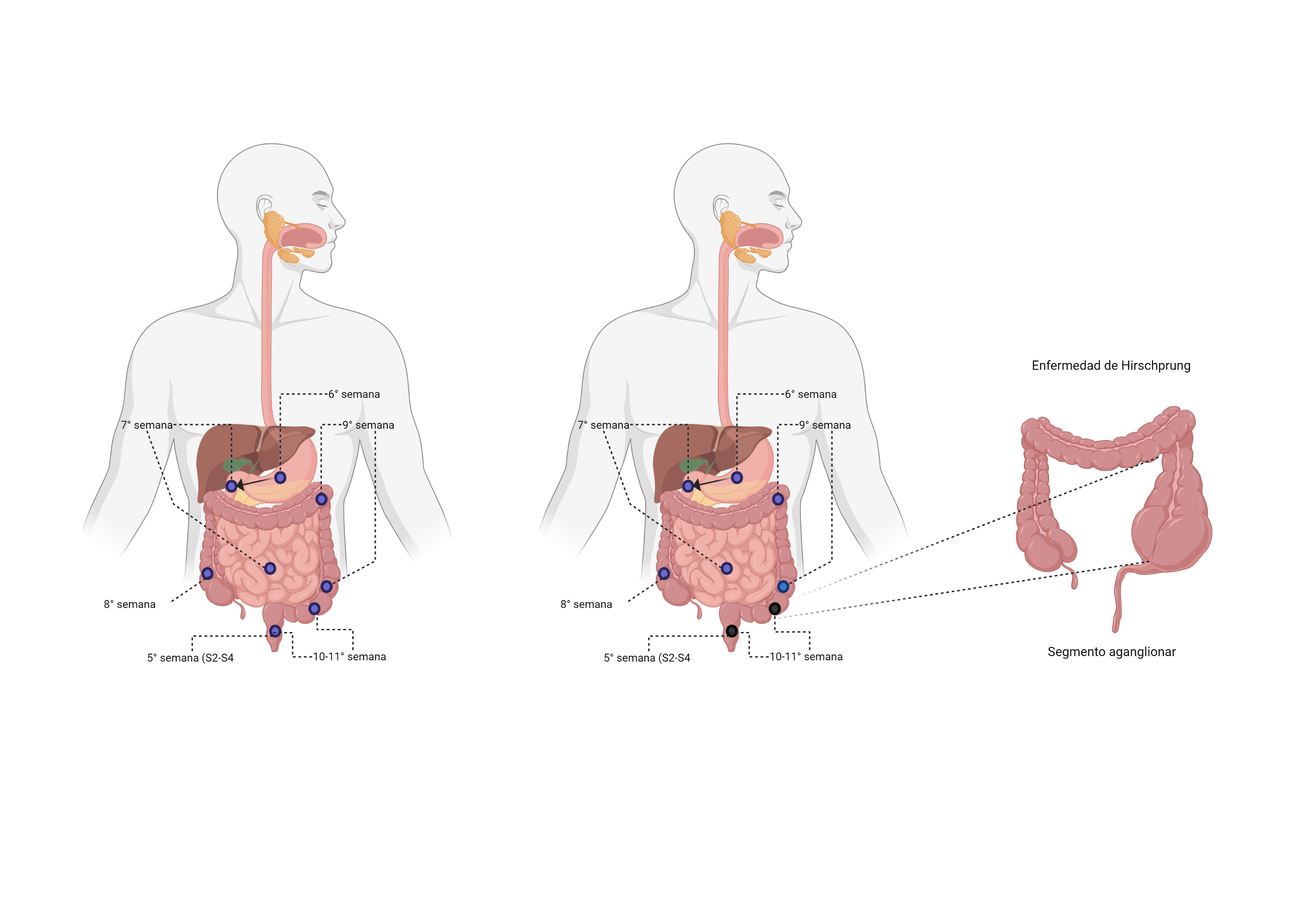
Hirschsprung's disease was described by the Danish pediatrician Harald Hirschsprung in 1888. It is the most common congenital enteric neuropathy, with a lack of relaxation of the enteric muscle, with subsequent intestinal obstruction. Its etiopathogenesis is given by aganglionosis in the digestive tract, mainly affecting the rectosigmoid region. Thus, keeping the internal anal sphincter contracted. It is classified into four types: short segment, the most common; long segment, ultrashort segment, and aganglionosis coli. The clinical presentation frequently begins in the neonatal period. The classic triad consists of abdominal distention, absence of meconium in the first 24 to 48 hours of life, and bilious vomiting with intolerance to the oral route. The diagnostic approach is performed by abdominal X-rays, contrast enema, or rectal manometry. The gold standard test is the rectal biopsy, which is considered positive if there are no ganglion cells in the myenteric and submucosal plexus of the colon. The initial management of the disease is based on intravenous fluid resuscitation, broad-spectrum antibiotics to prevent enterocolitis and bacterial translocation, decompression with a nasogastric tube, and colonic lavage. The definitive treatment is colonic resection of the affected segment. The main postoperative complications are perianal excoriation, constipation, dirt, diarrhea, fecal incontinence, and enterocolitis.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Schäppi MG, Staiano A, Milla PJ, Smith VV, Dias JA, Heuschkel R, et al. A Practical Guide for the Diagnosis of Primary Enteric Nervous System Disorders: J Pediatr Gastroenterol Nutr. noviembre de 2013;57(5):677-86. DOI: https://doi.org/10.1097/MPG.0b013e3182a8bb50
Tabbers MM, DiLorenzo C, Berger MY, Faure C, Langendam MW, Nurko S, et al. Evaluation and treatment of functional constipation in infants and children: evidence-based recommendations from ESPGHAN and NASPGHAN. J Pediatr Gastroenterol Nutr. 2014;58(2):258–74. DOI: https://doi.org/10.1097/MPG.0000000000000266
Moore SW. Advances in understanding functional variations in the Hirschsprung disease spectrum (variant Hirschsprung disease). Pediatr Surg Int. 2017;33(3):285-98. DOI: https://doi.org/10.1007/s00383-016-4038-3
Torre-Mondragón L. Enfermedad de Hirschsprung. Mitos y realidades a 120 años de su descripción. Acta Pediatr Mex. 2008;29(3):139-146.
Carro Gabriela, Ormaechea Martín, Silva Ema Da, Juambeltz Carlos. Enfermedad de Hirschsprung: resultados del tratamiento quirúrgico en el Hospital Pediátrico Pereira Rossell. Arch. Pediatr. Urug. 89( 3 ): 158-164.
Sajjad N, Hilal K, Khandwala K, Arshad M, Uddin N. Usefulness of delayed films of contrast enema for detecting Hirschsprung’s disease. Cureus. 2019;11(12):e6339. DOI: https://doi.org/10.7759/cureus.6339
Butler Tjaden NE, Trainor PA. The developmental etiology and pathogenesis of Hirschsprung disease. Transl Res. 2013;162(1):1-15. DOI: https://doi.org/10.1016/j.trsl.2013.03.001
Amiel J, Lyonnet S. Hirschsprung disease, associated syndromes, and genetics: a review. J Med Genet. 2001;38(11):729–39. DOI: https://doi.org/10.1136/jmg.38.11.729
Kroll-Wheeler L, Wilson AM. Educational Case: Hirschsprung Disease. Acad Pathol. 1 de enero de 2019;6:237428951989308. DOI: https://doi.org/10.1177/2374289519893088
Hackam D, Grikscheit T, Wang K, Upperman J, Ford H. Chapter 39: Pediatric Surgery. In: Andersen D, Dunn D, Hunter J, ed. by. Schwartz’s principles of surgery 11th ed. Mc Gram Hill; 2019.
Moore SW. Total colonic aganglionosis in Hirschsprung disease. Semin Pediatr Surg. 2012;21(4):302-9. DOI: https://doi.org/10.1053/j.sempedsurg.2012.07.004
Raveenthiran V. Knowledge of ancient Hindu surgeons on Hirschsprung disease: evidence from Sushruta Samhita of circa 1200-600 bc. J Pediatr Surg. 2011;46(11):2204-8. DOI: https://doi.org/10.1016/j.jpedsurg.2011.07.007
Das K, Mohanty S. Hirschsprung Disease — Current Diagnosis and Management. Indian J Pediatr. 2017;84(8):618-23. DOI: https://doi.org/10.1007/s12098-017-2371-8
Mc Laughlin D, Puri P. Familial hirschsprung’s disease: a systematic review. Pediatr Surg Int. 2015;31(8):695-700. DOI: https://doi.org/10.1007/s00383-015-3730-z
Moore SW. Advances in understanding the association between Down syndrome and Hirschsprung disease (DS–HSCR). Pediatr Surg Int. 2018;34(11):1127-37. DOI: https://doi.org/10.1007/s00383-018-4344-z
Villota D VA, Saldarriaga G W, Gómez C JF. Síndrome de Mowat-Wilson: caso clínico. Rev Chil Pediatría. 2012;83(4):371-6. DOI: https://doi.org/10.4067/S0370-41062012000400008
Coyle D, Puri P. Hirschsprung’s disease in children with Mowat–Wilson syndrome. Pediatr Surg Int. 2015;31(8):711-7. DOI: https://doi.org/10.1007/s00383-015-3732-x
Moore SW, Maluleke T, El Hosny AA. Is Hirschsprung disease a purely neurological condition? A study of the Actin G2 smooth muscle gene in Hirschsprung disease. J Pediatr Surg. 2019;54(10):2028-31. DOI: https://doi.org/10.1016/j.jpedsurg.2019.01.069
Jiménez, J. and Fernandez, L., n.d. Enfermedad de Hirschsprung. AEPED, pp.47-52.
Wetherill C, Sutcliffe J. Hirschsprung disease and anorectal malformation. Early Hum Dev. 2014;90(12):927-32. DOI: https://doi.org/10.1016/j.earlhumdev.2014.09.016
Muise ED, Cowles RA. Rectal biopsy for Hirschsprung’s disease: a review of techniques, pathology, and complications. World J Pediatr. 2016;12(2):135-41. DOI: https://doi.org/10.1007/s12519-015-0068-5
Tam PKH, Chung PHY, St Peter SD, Gayer CP, Ford HR, Tam GCH, et al. Advances in paediatric gastroenterology. The Lancet. 2017;390(10099):1072-82. DOI: https://doi.org/10.1016/S0140-6736(17)32284-5
Cathia Selman; Constanza Alzola Internas 7° año, Facultad de Medicina, Universidad de Chile. Enfermedad de Hirschprung: Avances en el diagnóstico. Rev. Ped. Elec. 2016;13(2):13-18.
Westfal ML, Goldstein AM. Pediatric enteric neuropathies: diagnosis and current management. Curr Opin Pediatr. 2017;29(3):347-53. DOI: https://doi.org/10.1097/MOP.0000000000000486
Massardo V Teresa, Jaimovich F Rodrigo, Rodríguez T J. Carlos, Azolas A Cristián, Saavedra S José, Lillo G Ricardo et al . Tromboembolismo pulmonar en lactante menor, portadora de enfermedad de Hirschsprung: caso clínico. Rev. chil. radiol. 2005;11(1): 32-35. DOI: https://doi.org/10.4067/S0717-93082005000100008
Alberto Peña. Enfermedad de Hirschsprung Los avances y las preguntas no contestadas. Cir. Pediatr. 2002; 15: 46-47.
Suita S, Taguchi T, Ieiri S, Nakatsuji T. Hirschsprung’s disease in Japan: analysis of 3852 patients based on a nationwide survey in 30 years. J Pediatr Surg. enero de 2005;40(1):197-202. DOI: https://doi.org/10.1016/j.jpedsurg.2004.09.052
PÉREZ BILLI LUIS E, BENEDICTTI JUAN L, GUTIÉRREZ CARMEN, GALIANA HORACIO GUTIÉRREZ. Enfermedad de Hirschsprung con afectación total del colon: primer caso nacional con la técnica quirúrgica de Lester Martin modificada. Arch. Pediatr. Urug. 2001;72(1): 34-37.
Nakamura H, Lim T, Puri P. Inflammatory bowel disease in patients with Hirschsprung’s disease: a systematic review and meta-analysis. Pediatr Surg Int. 2018;34(2):149-54. DOI: https://doi.org/10.1007/s00383-017-4182-4
Green HL, Rizzolo D, Austin M. Surgical management for Hirschsprung disease: A review for primary care providers. J Am Acad Physician Assist. 2016;29(4):249. DOI: https://doi.org/10.1097/01.JAA.0000481397.68475.41
Ciriza-de-los-Ríos, Constanza, Mínguez, Miguel, Remes-Troche, José-María, & Lacima, Glòria. Manometría anorrectal de alta resolución y de alta definición: redescubriendo la función anorrectal. Revista Española de Enfermedades Digestivas. 2018;110(12):794-805. DOI: https://doi.org/10.17235/reed.2018.5705/2018