Acute lobar nephronia in the pediatric patient. Case report
Main Article Content
Abstract
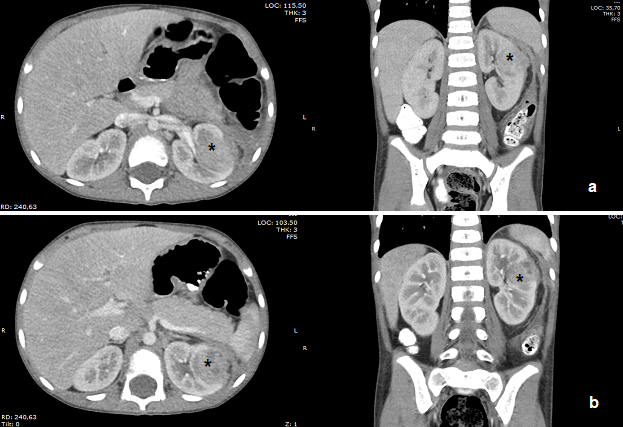
Background: Acute focal nephritis is a renal inflammation of bacterial origin, without liquefaction, that affects one or more renal lobes. This entity is underdiagnosed, and few cases are described in the literature. Its recognition is essential due to its relationship with urosepsis and renal scars. It can simulate a kidney tumor. It is associated with malformations of the urinary tract. Diagnostic images are of great value, with ultrasound and tomography being the images of choice. Treatment consists of antibiotic therapy, with generally good evolution. Case report: Male patient, six years old, with two weeks of daily fever, without other symptoms. Regular physical exam. Complete blood count with leukocytosis and neutrophilia. The abdominal ultrasound showed a non-specific renal lesion in the upper left pole. Contrast-enhanced abdominal tomography showed a heterogeneous left renal tumor with poorly defined borders, compromising the renal cortex, capsule, and perirenal space, without calcifications, collections, and evident tumor characteristics, without enhancement with contrast medium. MRI of the abdomen contrasted with a lesion compatible with an inflammatory process. Management with amikacin, cephalothin, and clindamycin for three weeks, with good evolution. Control images with a decreased lesion. Conclusion: Acute focal nephritis is a rare entity in pediatrics. Its recognition is essential due to its impact on renal function. The images of choice are ultrasound and CT. Antibiotic management is recommended for three weeks, the study of associated urinary malformations, ultrasound follow-up, and DMSA scintigraphy to evaluate scars.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Rosenfiled A, Gilckman M, Taylor K, Crade M, Hodson J. Acute focal bacterial nephritis (acute lobar nephronia). Radiology. 1979; 132(1):553-61. DOI: https://doi.org/10.1148/132.3.553
Vergara-Espitia A, Gallo-Urina K, Landinez-Millán G, Camacho-Moreno G, Lozano-Triana C. Nefronía lobar aguda en un niño: reporte de caso. Rev. Fac. Med. 2015; 63(2):321-4. DOI: https://doi.org/10.15446/revfacmed.v63n2.47501
Vijayakumar M, Prahlad N, Nandhini G, Prasad N, Muralinath S. Child with acute lobar nephronia. Indian J Nephrol. 2010; 20(3):162-5. DOI: https://doi.org/10.4103/0971-4065.70847
Cheng C, Tsau Y, Chang C, Chang Y, Kuo C, Tsai I, et al. Acute lobar nephronia is associated with a high incidence of renal scarring in childhood urinary tract infections. Pediatr Infect Dis J. 2010; 29(7):624-8. DOI: https://doi.org/10.1097/INF.0b013e3181d8631a
Piñera C, Loyola F, Hernández P. Nephronia in pediatrics: part of the spectrum of upper urinary tract infections. Clinical cases and review of the literature. Rev Chilena Infectol. 2015; 32(5):564-8. DOI: https://doi.org/10.4067/S0716-10182015000600011
Cano F, Strodthoff P, Muñoz O. Nefritis Aguda Focal. Caso Clínico. Rev. chil. pediatr. 2010; 81(3):247-252. DOI: https://doi.org/10.4067/S0370-41062010000300008
Klar A, Hurvitz H, Berkun Y, Nadjari M, Blinder G, Israeli T, et al. Focal bacterial nephritis (lobar nephronia) in children. J Pediatr. 1996; 128(6):850-3. DOI: https://doi.org/10.1016/S0022-3476(96)70340-2
Granados A, Espino M, Gancedo A, Albillos J, Álvarez-Cortinas J, Molina C. Nefronía focal aguda bacteriana: diagnóstico, tratamiento y evolución. An Pediatr (Barc). 2007; 66(1):84-6. DOI: https://doi.org/10.1157/13097366
Cheng C, Tsau Y, Lin T. Effective Duration of Antimicrobial Therapy for the Treatment of Acute Lobar Nephronia. Pediatrics. 2006; 117(1):84-9. DOI: https://doi.org/10.1542/peds.2005-0917