Pediatric suicide attempt and admission to the Intensive Care Unit, before and after the pandemic, at a university hospital in Boyacá, Colombia
Main Article Content
Abstract
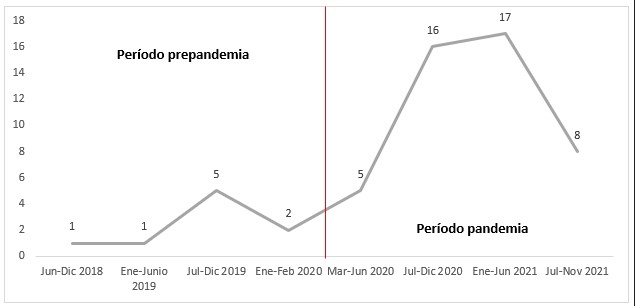
Introduction: The COVID-19 pandemic has had a profound impact on the mental health of children and adolescents, considering that confinement abruptly interrupted their school and social environment, experiencing sensations such as anxiety, irritability, and sad mood, which has been related to the increased in suicide attempts. Objective: to clinically and socio-demographically characterize the pediatric population that suffered a suicide attempt and was admitted to the intensive care unit before and during the pandemic. Methods: Descriptive cross-sectional study. All patients between 0 and 18 years of age admitted to the intensive care unit due to a suicide attempt were included. Results: 55 patients were included, of whom 82.1% attempted suicide during the COVID-19 pandemic. The adolescents and the female sex were the most affected. Most suicide attempts occurred at home, with intoxication being the most frequent mechanism and medications the most used substance. Gastric lavage was the most frequent treatment, and only one suicide attempt was fatal. Conclusion: During the new coronavirus pandemic, the number of suicide attempts in the pediatric population increased. Adolescents and females were the most frequently affected by suicide attempts, drugs being the substance they use the most due to the ease of access within the home.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Pantoja-Chamorro FI, Rodríguez-Villota AX, Urbano-Urbano J, Cabrera-Bravo N. Epidemiología del intento suicida en menores de 18 años atendidos en el Hospital Infantil los Ángeles, Pasto, Colombia. Universidad y Salud. 2018;21(1):19–26.
Cuesta-Revé D. Aspectos epidemiológicos del suicidio en adolescentes. Revista Mexicana de Pediatria. 2017;84(2):72–7.
World Health Organization. Prevención de la conducta suicida en la APS. Vol. 18, Revista Cubana de Medicina General Integral. 2002. 149–154.
Crosby A, Ortega L, Melanson C. Self - Directed Violence Surveillance Uniform definitions and recommended data elements. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. 2011. 91.
Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(4):386–405. DOI: https://doi.org/10.1097/01.CHI.0000046821.95464.CF
Cwik MF, O’Keefe VM, Haroz EE. Suicide in the pediatric population: screening, risk assessment and treatment. International Review of Psychiatry. 2020;32(3):254–64. DOI: https://doi.org/10.1080/09540261.2019.1693351
Zainum K, Cohen MC. Suicide patterns in children and adolescents: a review from a pediatric institution in England. Forensic Science, Medicine, and Pathology. 2017;13(2):115–22. DOI: https://doi.org/10.1007/s12024-017-9860-y
Instituto Nacional de Salud. Comportamiento de la vigilancia del intento de suicido en Colombia. Período epidemiológico III,2021. Boletin epidemiologico semanal. 2021;61(2):4518–26. DOI: https://doi.org/10.33610/23576189.2021.26
Meyers N, Friedman S, Anderson-Burnett SA. The Adolescent Mental Health Crisis in the Context of COVID-19: A Pediatric Resident Perspective. journal of adolescent health. 2021;69(January):672–5. DOI: https://doi.org/10.1016/j.jadohealth.2021.07.009
Hill RM, Rufino K, Kurian S, Saxena J, Saxena K, Williams L. Suicide ideation and attempts in a pediatric emergency department before and during COVID-19. Pediatrics. 2021;147(3). DOI: https://doi.org/10.1542/peds.2020-029280
Caycedo A, Arenas ML, Benítez M, Cavanzo P, Leal G, Guzmán YR. Características psicosociales y familiares relacionadas con intento de suicidio en una población adolescente en Bogotá́ - 2009. persona y bioética. 2010;14(2):205–13. DOI: https://doi.org/10.5294/pebi.2010.14.2.8
Benítez Camacho E. Suicidio: el impacto del Covid-19 en la salud mental. Revista de Medicina y Ética. 2021 Jan 4;32(1):15–39. DOI: https://doi.org/10.36105/mye.2021v32n1.01
Jiménez Quenguan M, Hidalgo Bravo J, Camargo Santacruz C, Dulce Rosero B. El intento de suicidio en la población pediátrica, una alarmante realidad. Revista Ciencias de la Salud. 2014;12(1):59–92. DOI: https://doi.org/10.12804/revsalud12.1.2014.05
Pantoja-Chamorro FI, Rodríguez-Villota AX, Urbano-Urbano J, Cabrera-Bravo N. Epidemiología del intento suicida en menores de 18 años atendidos en el Hospital Infantil los Ángeles, Pasto, Colombia. Universidad y Salud. 2018 Dec 21;21(1):19–26. DOI: https://doi.org/10.22267/rus.192101.136
Constanza S, Buitrago C, Alberto J, Parra C. Revisión Ideación y conductas suicidas en adolescentes y jóvenes.
Miranda-Mendizabal A, Castellví P, Parés-Badell O, Alayo I, Almenara J, Alonso I, et al. Gender differences in suicidal behavior in adolescents and young adults: systematic review and meta-analysis of longitudinal studies. Vol. 64, International Journal of Public Health. Springer International Publishing; 2019. p. 265–83. DOI: https://doi.org/10.1007/s00038-018-1196-1
Tamayo Cordoví A, Montes YE, Coto batista T, Sánchez Pérez YY. Factores de riesgo asociados a intento suicida en adolescentes. Unidad de cuidados intensivos pediátricos 2018-2019. Multimed. 2021;25(3).
Cortés Alfaro A, Suárez Medina R, Serra Larin S. Métodos y sustancias empleadas en la conducta suicida en adolescentes. Revista cubana de Medicina General Integral. 2019;35(4).
Hernández Loriga W, Salgado Rodríguez CA, Padrón Álvarez JE, Dorta Correa Y, Duardo Quintana ÁM, Larrionda Váldes N, et al. Intoxicaciones agudas exógenas en niños y adolescentes ingresados en cuidados intensivos pediátricos. Revista Cubana de Pediatría. 2020;92(2).
UNICEF España. Salud mental e infancia en el escenario de la covid-19 propuestas de UNICEF España. 2020 Jun.
Instituto Nacional de Salud. Boletín Epidemiológico semanal :Semana epidemiológica 35. 2020 Sep. DOI: https://doi.org/10.33610/23576189.2020.35
Lopez-Serrano J, Díaz-Bóveda R, González-Vallespí L, Santamarina-Pérez P, Bretones-Rodríguez A, Calvo R, et al. Psychological impact during COVID-19 lockdown in children and adolescents with previous mental health disorders. Revista de Psiquiatria y Salud Mental. 2021.
Orri M, Galera C, Turecki G, Forte A, Renaud J, Boivin M, et al. Association of childhood irritability and depressive/anxious mood profiles with adolescent suicidal ideation and attempts. JAMA Psychiatry. 2018 May 1;75(5):465–73. DOI: https://doi.org/10.1001/jamapsychiatry.2018.0174