Diverticulitis in the sigmoid colon of a 9-year-old girl. Case report
Main Article Content
Abstract
Introduction: A true intestinal diverticulum is an extraluminal protrusion that includes all histological layers and is commonly congenital. Diverticulitis mainly affects elderly patients, especially those >60 years of age, and is very rare in pediatric patients.
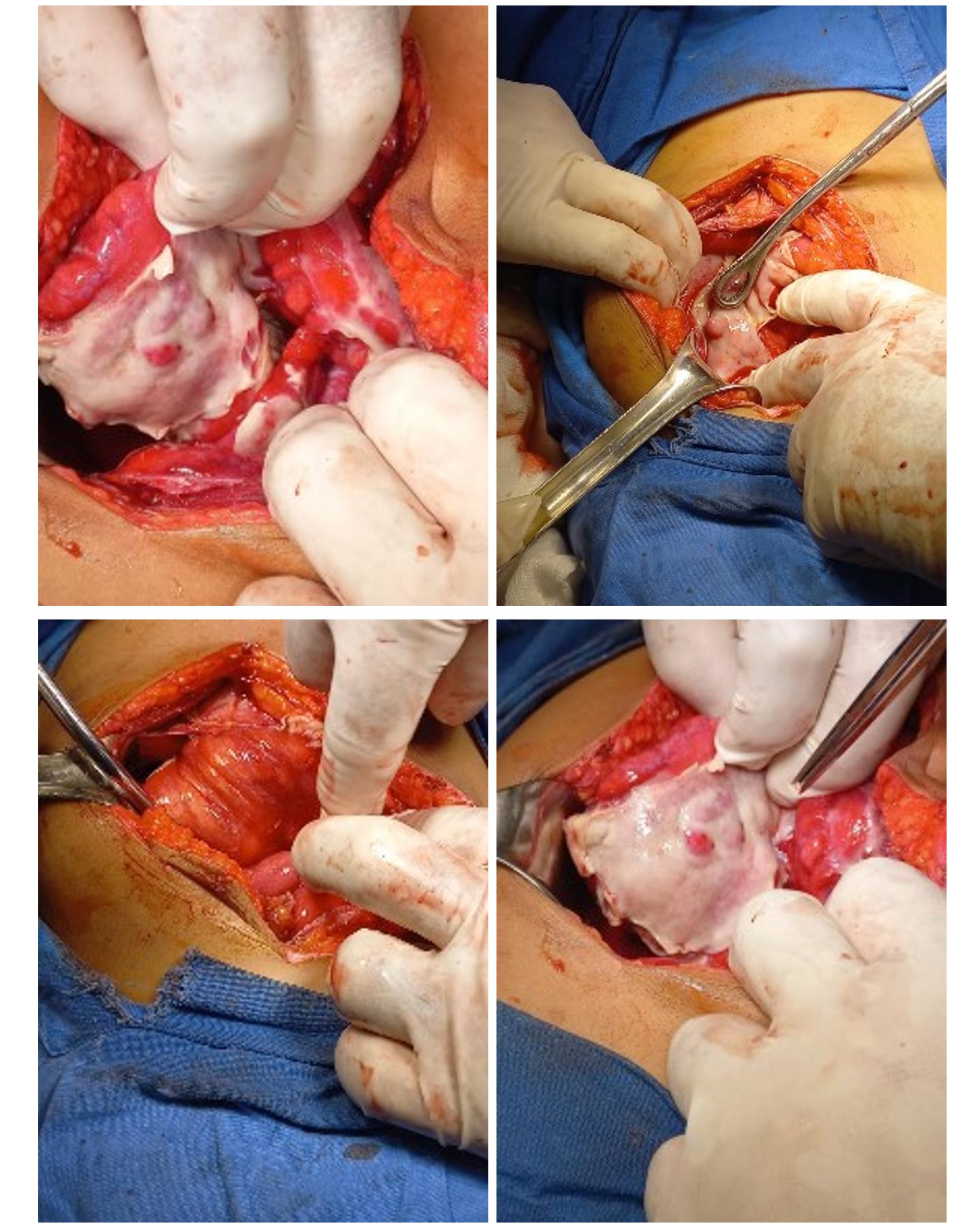
Case report: A case of a 9-year-old female patient is reported who arrives at the emergency room with generalized abdominal pain, fever, general malaise, positive rebound sign and leukocytosis. The diagnosis of acute appendicitis is established, so he is scheduled for laparoscopy. During the transoperative period, debris was found in all sites and cavities with fibrin and the presence of multiple diverticula from the sigmoid to the splenic flexure, with retractile mesenteritis. The sigmoid was resected, a Hartman-type colostomy was added, and antibiotic therapy was added, with adequate evolution.
Conclusions: Diverticulitis in children is often confused with acute appendicitis, its most frequent presentation in children is cecal diverticulitis, which is associated with genetic alterations of the connective tissue such as cystic fibrosis, Marfan syndrome, Ehlers-Danlos syndrome and syndrome of Williams-Beuren.
Downloads
Article Details

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Creative Commons
License Attribution-NonCommercial-ShareAlike 4.0 International (CC BY-NC-SA 4.0)
You are free to:
Share - copy and redistribute the material in any medium or format.
Adapt - remix, transform, and build upon the material The licensor cannot revoke these freedoms as long as you follow the license terms.
• Attribution — You must give appropriate credit, provide a link to the license, and indicate if changes were made. You may do so in any reasonable manner, but not in any way that suggests the licensor endorses you or your use.
• NonCommercial — You may not use the material for commercial purposes.
• ShareAlike — If you remix, transform, or build upon the material, you must distribute your contributions under the same license as the original.
• No additional restrictions — You may not apply legal terms or technological measures that legally restrict others from doing anything the license permits.
References
Strate LL, Morris AM. Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology. 2019; 156 (5): 1282-1298. https://doi.org/10.1053/j.gastro.2018.12.033. DOI: https://doi.org/10.1053/j.gastro.2018.12.033
Raña-Garibay R, Salgado-Nesme N, Carmona-Sánchez R, Remes-Troche JM, Aguilar-Carrera J, Alonso -Sánchez L, et al. Consenso mexicano sobre el diagnóstico y tratamiento de la enfermedad diverticular del colon. Rev Gastroenterol Mex. 2019; 84 (2): 220-240. https://doi.org/10.1016/j.rgmx.2019.01.002. DOI: https://doi.org/10.1016/j.rgmx.2019.01.002
Afzal NA, Thomson M. Diverticular disease in adolescence. Best Pract Res Cl Ga. 2002; 16 (4): 621-634. https://doi.org/10.1053/bega.2002.0303. DOI: https://doi.org/10.1053/bega.2002.0303
TingTing Z, RuiYun Z, Peng C, Jie Z, Jian L, Hao W, et al. Clinical analysis of 116 children with Meckel’s diverticulum and review of the literatura. Research Square 2023. PREPRINT. https://doi.org/10.21203/rs.3.rs-3420902/v1. DOI: https://doi.org/10.21203/rs.3.rs-3420902/v1
Kamal MU, Baiomi A, Balar B. Acute Diverticulitis: A Rare Cause of Abdominal Pain. Gastroenterol Res. 2019; 12 (4): 203–207. https://doi.org/10.14740/gr1166. DOI: https://doi.org/10.14740/gr1166
Santohigashi K, Lewis K, Ho CH. It's Not Appendicitis!. J Pediatr. 2016; 170: 340-341. https://doi.org/10.1016/j.jpeds.2015.11.027. DOI: https://doi.org/10.1016/j.jpeds.2015.11.027
Valenzuela-Salazar C, Orozco-Tapia LM, Blankenagel EC, Gallardo-Ramírez MA, Miguel Blas-Franco, Luis Eduardo Cárdenas-Lailson. Diverticulitis de sigmoides en adolescente: Reporte de caso. Cir Cir. 2013; 81 (5): 445-449.
Gómez-Sánchez J, Ramos-Sanfiel J, Zurita-Saavedra M, Ubiña-Martinez JA, García-Martinez MÁ, Castro-Monedero P, et al. Situaciones especiales en el tratamiento de la enfermedad diverticular: Enfermedad multifocal, divertículo gigante, diverticulitis en colon derecho y diverticulitis en pacientes inmunosuprimidos. Cir Andal. 2021; 32 (4): 507-513. https://doi.org/10.37351/2021324.13. DOI: https://doi.org/10.37351/2021324.13
Hatakeyama T, Okata Y, Miyauchi H, Hisamatsu C, Nakatani T, Nakai Y, et al. Colonic diverticulitis in children: A retrospective study of 16 patients. Pediatr Int. 2021; 63 (12): 1510-1513. https://doi.org/10.1111/ped.14693. DOI: https://doi.org/10.1111/ped.14693
Santin BJ, Prasad V, Caniano DA. Colonic diverticulitis in adolescents: an index case and associated síndromes. Pediatr Surg Int. 2009; 25 (10): 901–905. https://doi.org/10.1007/s00383-009-2472-1. DOI: https://doi.org/10.1007/s00383-009-2472-1
Aktay A, Segura AD, Oldham KT, Kugathasan S. Diffuse diverticulosis of colon with spontaneous perforation in a child. J Pediatr Gastroenterol Nutr. 1999; 29 (4): 521. DOI: https://doi.org/10.1097/00005176-199910000-00154
Bartel M, Burnett C, Barnes D. Sigmoid Diverticulitis in an Obese Pediatric Patient Without Genetic Predisposition. JPGN Reports. 2021; 2 (2): 78. https://doi.org/10.1097/PG9.0000000000000078. DOI: https://doi.org/10.1097/PG9.0000000000000078
Lee ZW, Albright EA, Brown BP, Markel TA. Congenital cecal diverticulitis in a pediatric patient. J Pediatr Surg Case Rep. 2021; 72: 101929. https://doi.org/10.1016/j.epsc.2021.101929. DOI: https://doi.org/10.1016/j.epsc.2021.101929